by Nathan Lucs, PT, DPT
Pain is a complex and inevitable fact of life. At some point or another we will all experience it. The pain experience is helpful as a guide to avoid further injury when experiencing an acute tissue injury, but what happens when it persists beyond tissue healing?
Pain does not have to be solely due to acute tissue or emotional injury. It can also be a reaction to POTENTIAL tissue or emotional damage. You see, the interpretation of pain is constructed in the brain, which means it doesn’t necessarily have to be provoked by a physical or emotional stimulus outside of the brain. This, in part, is why pain can persist beyond tissue healing.
How can I improve my pain experience and manage it?
One way you can improve and manage it is through education. Learning and understanding the pain science, physiology of pain, has been shown to reduce the pain experience and prevent catastrophizing. So reading this article and comprehending it alone has the potential to decrease your pain experience.
Let’s dive in to some education of terms and analogies to help paint a picture of a simplified version of the pain experience. First off, understand that there is no such category as “pain receptors” in the nerves that go out into your body from the spinal cord and return information. Instead, there are nerves that transmit uncomfortable sensations back to your brain that may or may not be injurious for the tissue it innervates. These nerves are called nociceptors. Then your mind interprets this as pain or brushes it off as something unimportant. A commonly used illustration can be explained like this: if you break your ankle and fall into the street, and that’s all you have to think about, then you likely will fall to the ground and lay there in agonizing pain. On the other hand, if you break your ankle and you have a bus heading your way, then you are likely to ignore the nociceptive inputs and get out of the way. In this case, it is more important to move than to interpret sensation of the irritated tissue at that time. Context is key to the pain experience. Nociceptive inputs from the body can be interpreted as pain, or can be brushed off as unimportant, annoying sensations only with the brain’s involvement. The resultant interpretation can be, in part, influenced by the context of the situation and knowledge of the physiology of pain.
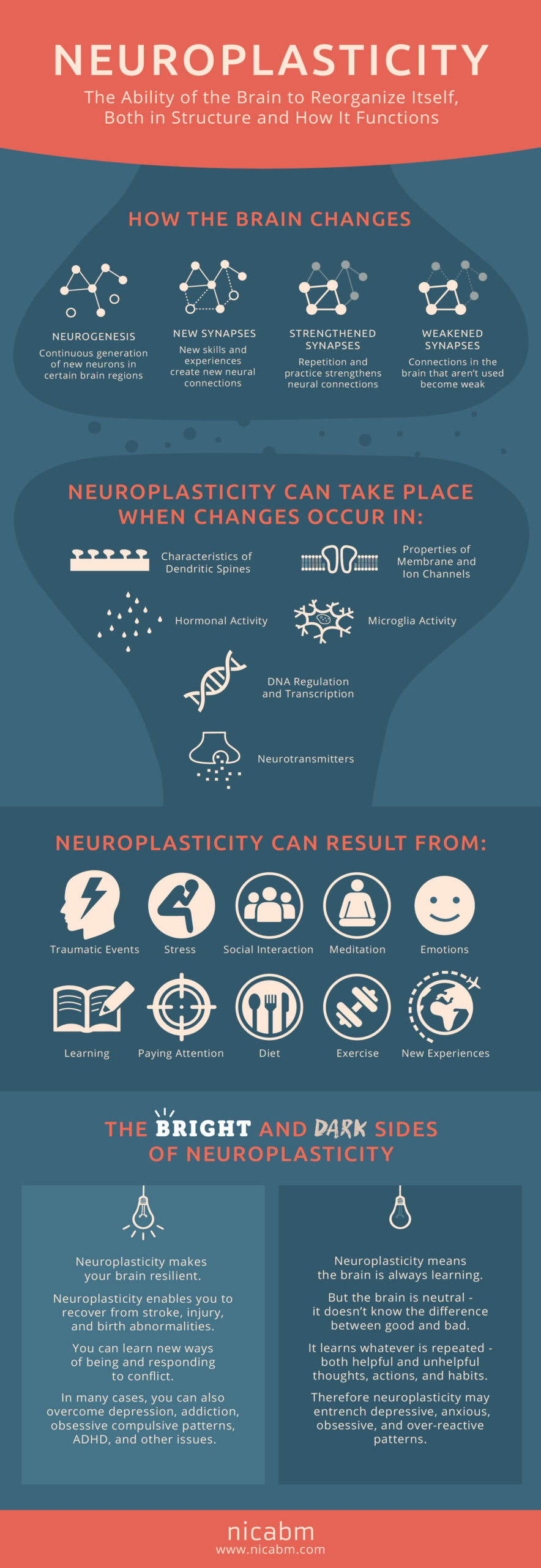
Additionally, the brain and nervous system outside of it are plastic, meaning they can change or essentially become rewired in a positive or negative way. When pain persists past tissue damage, rewiring (also known as neuroplasticity) can occur both in the brain and the nervous system outside of it. Changes in neural sensitivity through rewiring can lead to a perception of pain that is not equal to the amount of tissue injury, which can lead to increased fear (the thought of potential tissue injury), decreased physical activity, and more pain.1 This is when the perception of pain can become maladaptive. Think of it like an alarm system, you want it to be sensitive enough to tell you when someone is breaking in, but don’t want it to be so sensitive that (in the spirit of fall) a leaf sets it off. In this analogy, the nervous system is the alarm system, someone breaking in is an acute injury in which tissue damage occurs, and the leaf is common every day movements after the tissue damage has been resolved. We want an alarm system that is sensitive enough for acute injuries, yet resilient enough to allow for every day movement in the absence of tissue injury. One way to build a resilient alarm system is through movement and exercise.
Exercise is an innate pain killer! Aerobic exercise specifically stimulates endorphin release. It has been shown that a 6 mile run can produce endorphins equivalent to 10 mg of morphine. To put that into context, people typically get 2-4 mg of IV morphine for maintenance of acute pain in the ER.4 Now, I understand some of you might be saying to yourself, “I don’t want to run 6 miles, is there any other way to receive those benefits?” Well, there is great news because it just takes 10 minutes of moderate intensity aerobic exercise to produce an analgesic effect. Physical therapists can help with exercise modification and determining a graded exposure to exercise leading to an intensity that is right for you. (See the infographic provided by the ACSM for information on how to reach moderate intensity exercise if you are able.)
If you are interested in how you might benefit from exercise, feel free to reach out to us online or by calling 866-588-0230.
Sources
- Puentedura EJ, Louw A. A neuroscience approach to managing athletes with low back pain. Phys Ther Sport. 2012;13(3):123-133. doi:10.1016/j.ptsp.2011.12.001
- Van Oosterwijck J, Meeus M, Paul L, et al. Pain physiology education improves health status and endogenous pain inhibition in fibromyalgia: a double-blind randomized controlled trial. Clin J Pain. 2013;29(10):873-882. doi:10.1097/AJP.0b013e31827c7a7d
- Janal MN, Colt EW, Clark WC, Glusman M. Pain sensitivity, mood and plasma endocrine levels in man following long-distance running: effects of naloxone. Pain. 1984;19(1):13-25. doi:10.1016/0304-3959(84)90061-7
- Lexicomp. (n.d.). Morphine: Drug information. UpToDate. Retrieved October 25, 2020, from https://www.uptodate.com/contents/morphine-drug-information#F50711535
- Hoffman MD, Shepanski MA, Mackenzie SP, Clifford PS. Experimentally induced pain perception is acutely reduced by aerobic exercise in people with chronic low back pain. J Rehabil Res Dev. 2005;42(2):183-190. doi:10.1682/jrrd.2004.06.0065